February 2025 - 2
Author: Dr Eamonn Fahy
A 65-year-old male has recently moved interstate and attends your practice. He had previously been diagnosed with primary open angle glaucoma and was started on latanoprost drops for both eyes.
Pre-treatment intraocular pressures (IOP) were 21 mmHg in both eyes. IOP is now 14 mmHg in both eyes. Central corneal thickness is 498 µm right eye and 526 µm left eye. His best corrected visual acuity is 6/9 in both eyes. He describes gradual reduction in his vision over time. You perform visual field and OCT testing for him.
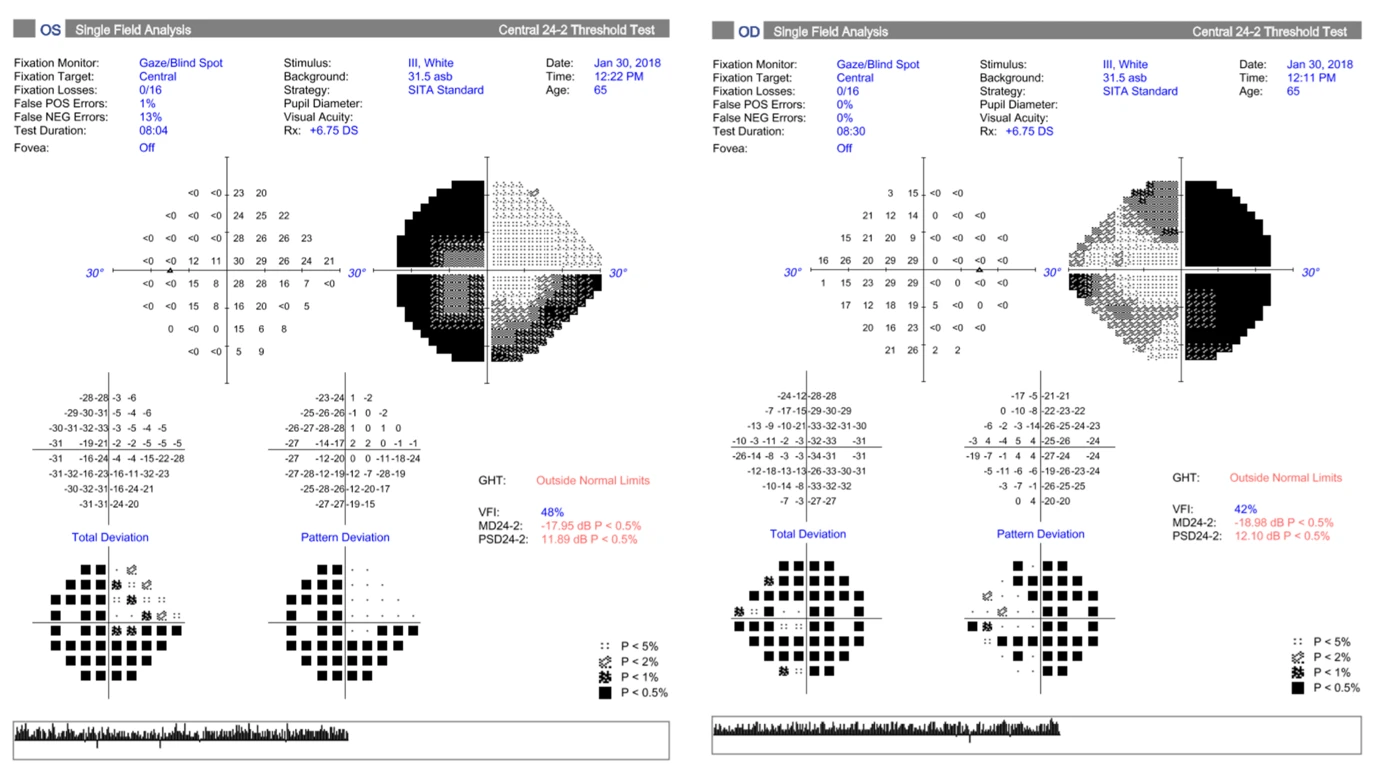
Figure 2 - Visual fields
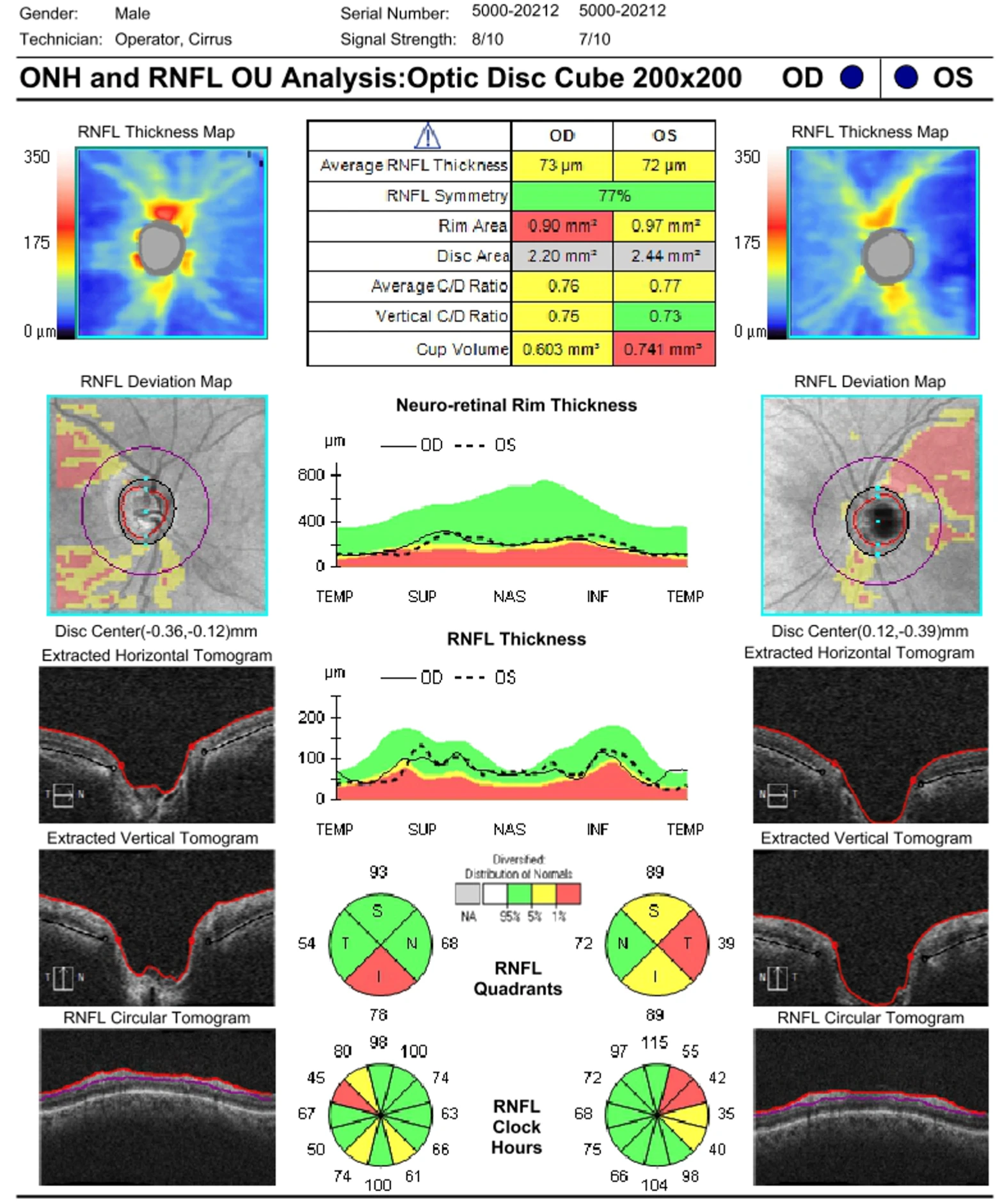
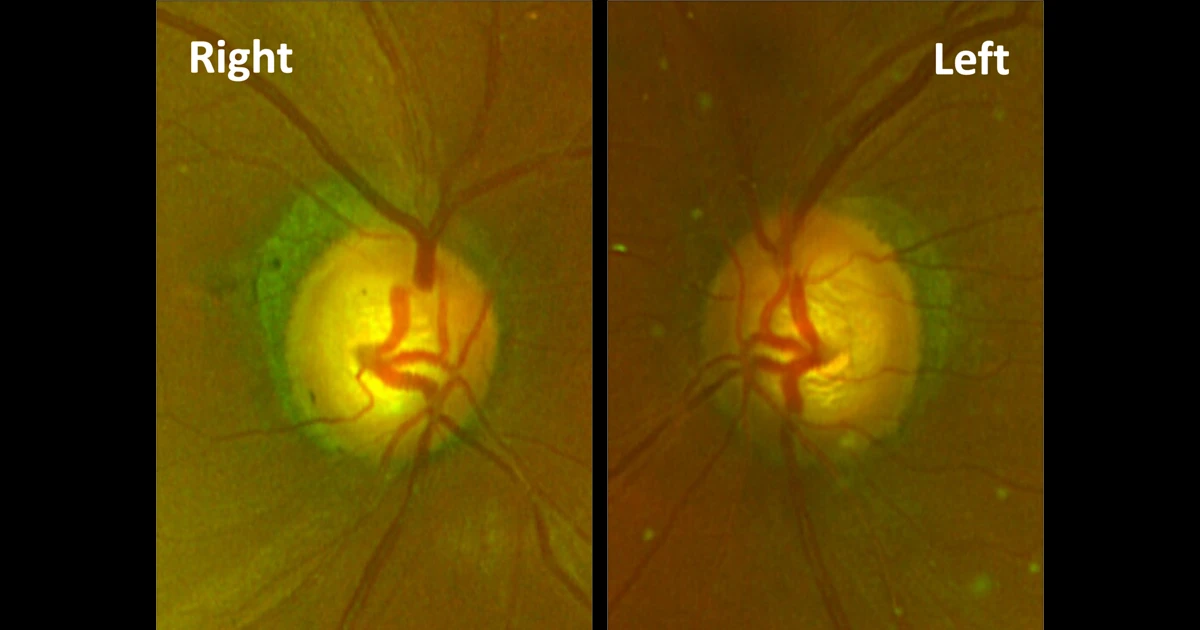
Figure 3 - ONH and RNFL
Based on the information provided, what is the next best step for this patient?
A - Continue to monitor his visual fields
Oops! Try again
B - Routine referral to an ophthalmologist for glaucoma follow up
Oops! Try again
C - Urgent referral to an ophthalmologist for assessment and neuroimaging
CORRECT!
D - Refer to GP for sleep studies
Oops! Try again
Answer C
This case of a pituitary tumour was originally diagnosed as glaucoma. The visual fields show bitemporal hemianopia. Visual field interpretation is made more difficult by the fact that the defect crosses the vertical midline on the pattern deviation. In this patient there may also be concurrent glaucoma, however the greyscale clearly demonstrates bitemporal hemianopia which respects the midline for the most part. Given the clinical presentation and visual fields, a priority referral to an ophthalmologist is indicated. CT or MRI neuroimaging will be required to confirm the diagnosis.
In the case above, an important screening test was left out, and that is colour vision. This patient had Ishihara testing of 9/17 in the right eye and 11/17 in the left eye. This highlights colour vision as an important screening tool for new glaucoma patients. Glaucoma does not tend to affect colour vision, and reduced colour vision should raise suspicion for a non-glaucomatous optic neuropathy. Reduced visual acuity and a relative afferent pupillary defect (RAPD) should also raise suspicion for non-glaucomatous aetiology.
The appearance of the optic nerves are also atypical for glaucoma. The appearance fits with the pattern of ‘bow-tie’ atrophy, which is bilateral horizontal orientated optic atrophy, and can be associated with compressive chiasmal tumours. The visual field defect is more severe than what you would expect to see, relative to the appearance of the optic nerve and OCT. This is another clue that the aetiology of the visual field defect may be intracranial.